Name of the Scheme – National Health Mission
Department – Directorate of Higher Education
Scheme for : Individual and Institutions
Where to Apply : Directorate office
When to Apply : Anytime of the Financial Year.
- About the Scheme
National Rural Health Mission (NRHM) was launched in April 12, 2005 to address the health needs of the underserved rural population especially women, children and vulnerable sections of the society and to provide affordable, accessible and quality healthcare.
The National Urban Health Mission, (NUHM) was launched in May 2013 and was subsumed with NRHM as a sub-Mission of the overarching National Health Mission. (NHM). Many unique practices were encouraged like innovations in healthcare delivery practices, flexible financing to the states with strengthened monitoring and evaluation component for better health outcomes and health indicators of the states.
The vision of the NHM is the “Attainment of Universal Access to Equitable, Affordable and Quality health care services, accountable and responsive to people’s needs, with effective inter-sectoral convergent action to address the wider social determinants of health”.
NHM focuses on decentralized health planning, service delivery, creating knowledge hubs within district hospitals, strengthening secondary level care at district hospitals, expanding outreach services, improving community processes and behavior change communication, human resources development, public health management, and health management information systems. NHM particularly focuses on equity: prioritizing the health of tribal populations, those in LWE and urban poor. A key outcome of NHM is to reduce Out of Pocket expenditures. Health outcomes, output and process indicators are monitored through large scale surveys conducted periodically with evaluations, use of HMIS data, and periodic reviews done.
The main aim is to create a fully functional, decentralized and community owned system with greater inter- sectoral coordination so that wider social determinant factors affecting health of people like water, sanitation, nutrition, gender and education are also equally addressed.
2. National Rural Health Mission (NRHM)
2.1 Objectives, Goals and Key Strategies of the NRHM Major Strategies were incorporated for improving outreach of health services to public for greater synergy; decentralized planning and innovation in service delivery. The summary of objectives, goals and strategies are in Table 1:
Table 1: Objectives, Goals & Strategies of NRHM
| Objective | Goal | Strategic Changes |
| 1. Reduction in Infant Mortality Rate (IMR) and Maternal Mortality Rate (MMR 2. Population stabilization, gender and demographic balance | 1. Reduce IMR to 25/ 1000 live births 2. . Prevention and reduction of anaemia in women aged 15- 49 years 3. Reduce Total Fertility Rate (TFR) to 2.1 4. Reduce MMR to 1/ 1000 live births | 1. Strengthening infrastructure at all levels 2. Quality Monitoring of facilities as per Indian Public Health Standards ( IPHS) Standard 3. Decentralised planning with autonomy for local action 4. Institutional Mechanisms at all levels with autonomy 5. Induction of management specialist into Programme management Units 6. Centralized technical support unit- National Health Resource Centre and State Health Resource Centre (NHSRC and SHSRC) |
| 3. Achieve Universal access to public health services like women’s health, child health, water, sanitation & hygiene, immunization, and nutrition. 4. Promotion of healthy life styles | 1. Reduce household out –of-pocket expenditure on total health care expenditure | 1. Decentralised planning with autonomy for local action 2. Inter sector District Health Plan includes drinking water, sanitation, hygiene, nutrition Capacity- Building of Panchayati Raj institutions 3. Developing capacities for preventive health care at all levels |
| 5. Prevention and control of communicable and non- communicable diseases, including locally endemic diseases | 1. Prevent and reduce mortality and morbidity from communicable, non- communicable, injuries and emergency diseases 2. Reduce annual incidence and mortality from Tuberculosis by half 3. Reduce prevalence of Leprosy to <1/10000 population and incidence to zero in all districts 4. Annual Malaria incidence to be <1/1000 Less than 1 per cent microfilaria prevalence in all districts 5. Kala- Azar Elimination by 2015, <1case per 10000 population in all blocks | 1. Integrating vertical Health and Family Welfare programmes 2. Developing capacities for preventive health care at all levels 3. Reorienting Medical Education to Rural Health Issues |
| 6. Access to integrated comprehensive primary healthcare 7. Revitalization of local health traditions and mainstream AYUSH | 1. Reduce household out –of-pocket expenditure on total health care expenditure | 1. Promote ASHA healthcare service delivery 2. Health Plan for each village through VHNSC 3. Untied funds with flexi pools of funds 4. Effective and visible risk pooling and social health insurance 5. Promoting non-profit sector and PPP for achieving goals in underserved areas 6. Mainstreaming AYUSH and local health traditions |
2.2 Public Health Planning and Financing:
• Mapping of facilities and differential planning for districts/cities/blocks as per their health indicators
• Planning for full spectrum of health services
• Emphasis on quality assurance in delivery points
• Strengthening of Management with full time Mission Director, Director Finance and Programme Management support at all levels.
• Developing a separate and trained Public health cadre of professionals including doctors and nurses
2.3 Human Resource Strengthening in Health; Deployment and Development
• HR gaps met based on case load. Engagement of medical specialists, Medical professionals and nurses on contract based on need.
• HR accountability: Performance- based incentives and for working in difficult areas.
• Additional incentives to health professionals to serve in rural and remote areas
• Speedy recruitment to fill up vacancy, preferable decentralized.
• Amendments in medical college norms to increase availability of doctors
• Capacity building and training of staff at all levels.
| Health facility level | Population Covered in Plain areas | Difficult/ tribal & hilly areas | Staff Requirement |
| Sub centre | 1 per 5,000 population | 1 per 3,000 population | 3 |
| Primary Health Centre (PHC) | 1 per 30,000 population | 1 per 20,000 population | 15 |
| Community Health Centre (CHC) | 1 per 1,20,000 population | 1 per 80,000 population | 25 |
| District Hospital | 100 beds per 1,00,000 population | 60-70 |
2.4 Health Systems Strengthening
Funds are provided for up gradation of existing and construction of new infrastructure. High focus States spend up to 33 per cent and other States up to 25 per cent of their funds on infrastructure. Relevant Guidelines in Table 2:
Table 2: Guidelines for health facilities based on population norms
Facility type and time taken to reach by walk
| Facility Type Time taken for walking to facility from any habitation | |
| Sub centre( in hilly and desert states) | Within 30 min |
| PHC CHC | Within 30 min |
| With 2 hrs | |
| However, to ensure easy access, facilities can be created/ upgraded based on the ‘time to care’ approach. | |
The various sub- components of Health Systems Strengthening are as follows:
1. Construction of new buildings and renovation of existing ones.
Budget provisions available for construction, maintenance, carpentry, electrical, plumbing, sanitation, water provision etc. to fulfill the infrastructural gaps based of IPHS (Indian Public Health Standards) and existing structure.
2. Improving Sanitation & Hygiene in Public facilities: Kayakalp
Kayakalp initiative is a new initiative launched in 2015 under NHM, to inculcate the practice of hygiene, sanitation, effective waste management and infection control in public health facilities. It also includes recognition with Certificate of Commendation and Cash Awards of such public healthcare facilities that show extraordinary performance and compliance to protocols.
| Facility Type | Ranked Awards | Certificate of Commendation |
| DH, CHC & SDH PHC | 1st 50 lakh, 2nd 20 lakh | Rs 3 lakh |
| 1st 15 lakh, 2nd 10 lakh | Rs 1 lakh | |
| 2 lakh | Rs 50,000 |
3. Social Protection: Reducing Out of pocket expense:

A. Drugs: Free Drugs Service Initiatives
• Provisions for supply of essential drugs as per the defined Essential Drugs List (EDL), free of cost, to lower the out- of- pocket expenses of the patients.
• Centrally procurement of drugs for various programmes as Standard Treatment Guidelines (STG) per the EDL and Provision of local purchase of drugs and supplies at lower levels, if need arises.
Drugs & Logistic Support: Procurement and Supply Chain Management Systems
Drug Procurement System for public health facilities and E-procurement systems are very crucial for supply of essential drugs for JSSK and other programmes.
B. Diagnostics: Free Diagnostics Service Initiative
Under this programme, free diagnostics services (radiological & laboratory) are provided to patients free of charge, as per the level of the facility. (Refer Guidelines on Free Diagnostics Service Initiative.
C. Diet: Free good quality Diet
It is available to all inpatients including pregnant women.
D. Transport: Emergency Response System (ERS)/ Patient National Ambulance Services (NAS)
Transport Service/
These services are offered on cashless basis and are the pillars for providing free assured transport services to the patients as entitled by Janani Suraksha Yojana (JSY) and Janani Sishu Suraksha Karyakram (JSSK).
Many of these models have dedicated call centers attached to them. In Dial 108 model, approximately one ambulance is positioned for one lakh population, and each ambulance has a staff of three drivers and three paramedical emergency technicians, with two supervisors for every 15 vehicles.
Equipments: Biomedical Equipment Management and Maintenance Programme The comprehensive program includes detailed guidelines on the comprehensive medical equipment management and maintenance in a Public Private Partnership mode, its components, structure for partnerships and inventory mapping.
4. Outreach Services: Mobile Medical Units
Vehicles are used to improve outreach services and bring healthcare to the doorstep of especially in difficult terrain and remote areas. It may carry medical and paramedical personnel, drugs, supplies and laboratory and diagnostics equipment. The number of vehicles varies from State to State.
Reproductive, Maternal, New Born, Child Health and Adolescent (RMNCH+ A) Services
This programme was launched in 2013 to address increasing maternal and child health mortality, associated causes and to bring in improvement in access and utilisation of health care services by the vulnerable population. The sub- components of this Scheme are as follows:
A. Reducing Maternal Mortality Rate: Maternal Health
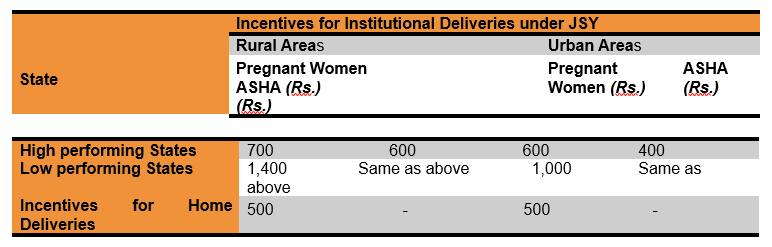
1. Incentivization: Janani Suraksha Yojana (JSY)
This scheme is for strengthening Maternal and Child Health Services wherein incentives are paid to all the pregnant women of both urban and rural areas for deliveries in public institutions. Incentives are given to all patients irrespective of their BPL status, so as to facilitate public institutional deliveries.
Table 4 a: Incentives for Institutional Deliveries under Janani Suraksha Yojana (JSY)
2. Free Patient Entitlements: Janani Sishu Suraksha Karyakram (JSSK)17
JSSK scheme ensures cashless delivery and C- section for pregnant women and management of sick neonates up to one year to prevent incurring high out- of- pocket expenses and exploitation by unwarranted people.
| Pregnant women | Sick newborns till 30 days after birth. |
| • Free and cashless delivery | • Free treatment |
| • Free C- Section | • Free drugs and consumables |
| • Free drugs and consumables | • Free diagnostics |
| • Free diagnostics | • Free provision of blood |
| • Free diet during stay in the health institutions | • Exemption from user charges |
| • Free provision of blood | • Free Transport from Home to Health Institutions |
| • Exemption from user charges | • Free Transport between facilities in case of |
| • Free transport from home to health institutions | referral |
| • Free transport between facilities in case of referral | • Free drop Back from Institutions to home |
| • Free drop back from Institutions to home after 48 | |
| hours stay | |
| Unit Price per case allocations to the hospital are Drugs & Consumable for Normal Deliveries- Rs.350/-, Drugs & Consumable for C- sections- Rs.1, 600/-, Diagnostic- Rs.200/-, Blood Transfusion- Rs.300/-, Transport (Referral transport inter facility) – Rs.250/. A separate account for this budget is maintained by the institutions. (Refer Guidelines on JSSK) | |
3. Strengthening infrastructure: Maternal and Child Health (MCH) Services
Under NHM, 100/50/30 bedded MCH wings are established to improve quality of care if the bed occupancy is more than 70 per cent. Such wings can be established in District Hospitals/ District Women’s Hospitals/ Sub- District Hospitals/CHC- First Referral Units (FRUs) to overcome the constraints of increasing caseloads and institutional deliveries at these facilities. (Refer: Maternal and Newborn Health Tool Kit, Nov 2013; MoHFW, GoI)
4. Reorienting Medical Education: Skill Labs
Skills Labs are established for competency based training and skill enhancement of healthcare providers for RMNCH+A services, both in- service and pre- service training. Thus reorient existing personnel and train students of ANM, GNM and midwifery courses.
5. Capacity Building: Dakshata Programme
It is the capacity building programme for service providers in labor room best practices during labor, delivery and post- partum.
6. Promotive Health : Mothers Absolute Affection (MAA)
It is a new initiative Programme for Promotion of Breast Feeding.
7. Improves access and Coverage: Safe Abortion Services
Medical Termination of Pregnancy (MTP) services are provided in FRUs, functional 24×7.
8. Improving access by PPP mode: Pradhan Mantri Surakshit Matritva Abhiyan(PMSMA)
Under the PMSMA, on the 9th of every month, pregnant ladies are given free health check- up including blood pressure, sugar level, Hemoglobin test, Blood test etc. and the required treatment in all government medical facilities. Private sector gynecologists are encouraged to voluntarily participate and provide antenatal checkup (ANC) services in these public health facilities.
9. NGOs Involvement: Gender Based Violence
ASHAs and clinical service providers are sensitized and trained to identify, counsel and refer such cases to higher centres, with the support of Non- Governmental Organisations (NGOs) and women support groups.
10. Monitoring and accountability of services: Maternal Death Review
The purpose of both Facility- Based Maternal Death Review (FBMDR) and Community- Based Maternal Death Review (CBMDR) is to identify the causes of maternal deaths and the gaps in service delivery in order to take corrective action.
B. Reducing Infant Mortality and Child Mortality Rate: New Born and Child Health
1. New born Care Services Programme
Table 5: Programmes under New- born Care Services Programme
| Newborn care services | Location | Services |
| New Born Care Corner New Born Stabilization Units (NBSU) | All Delivery points | Essential newborn care including resuscitation, Zero day immunization |
| CHCs/FRUs | Stabilization and referral of sick newborns. |
| Special New born Care Units (SNCUs) | DHs and tertiary care Management of sick new-borns hospitals |
2. Universal Immunization Programme (UIP) & Mission Indra dhanush
Under the routine immunization, children are given vaccines for the prevention of seven life- threatening diseases (Tetanus, Tuberculosis, Diphtheria, Pertussis, Measles, Polio and Hepatitis-B). Vitamin A dosages are also given with Measles. Tetanus Toxoid is provided to the pregnant women. These vaccinations are being organized by immunization sessions in all the hospitals, health centers, sub centers and anganwadi centers, during special vaccination weeks. Cold chain logistics are provided at all facilities. Surveillance of vaccine preventable diseases is integrated with Integrated Disease Surveillance Programme (IDSP). Name- based monitoring of both mother and children for vaccination are done through Mother and Child Tracking System (MCTS).
Mission Indradhanush: To strengthen and invigorate the Universal Immunization Programme (UIP) and achieve full immunization coverage for all children at a rapid pace, the Government of India (GoI) launched Mission Indradhanush in December 2014.25
Mission Indradhanush ensures that all children under the age of two years and pregnant women are fully immunized with all available vaccines. (Ref: Operational Guidelines for UIP and Operational Guidelines for Mission Indradhanush)
3. Rashtriya Bal Swasthya Karyakram (RBSK)26
The Purpose of RBSK is to improve the overall quality of life of children, 0- 18 years, through early detection & intervention of 4Ds i.e. Defect at birth, Diseases, Deficiencies, Developmental delays and disabilities. These will cover 38 identified health conditions through dedicated mobile health teams in every block in schools and Anganwadi centers. District Early Intervention Center (DEIC) is the setup for further screening, management support and referral to higher center.
4. Integrated Management of Common Childhood Illnesses(IMNCI)
Facilities for prevention, early detection and management of diarrhea, Pneumonia and Malaria
5. Nutritional Rehabilitation Centers (NRCs)
NRCs are set up in the health facilities, especially at DHs and FRUs for inpatient management of severely malnourished children, with counseling of mothers for proper feeding and regular follow up on discharge.
6. Monitoring: Child Death Review
Reporting and reviewing of child death under 5 years is a priority area.
C. Adolescent Health Programme
1. Rashtriya Kishor Swasthya Karyakram (RKSK) 27
Adolescent Friendly Health Services (AFHS) are present in district health facilities to provide counseling on sexual and reproductive health including menstrual hygiene, substance abuse, violence including domestic violence, mental health, injuries, non- communicable diseases and provide iron and folic acid tablets, condoms, pregnancy kits and Oral Contraceptive Pills (OCPs) through dedicated trained counselors.
D. Reducing Fertility Rate: Family Planning Services 28
For the purpose of encouraging family planning in the district, all PHCs, CHCs and DH services provide temporary and permanent family planning methods including male and female sterilization surgeries, Intrauterine Contraceptive Device (IUCD), Post- Partum Intrauterine Contraceptive Device (PPIUCD), Oral Contraceptive Pills (OCPs), Emergency Contraceptive Pills (ECPs), condoms and counseling services. In addition, outreach sterilization services are conducted in remote areas. A month long (in two phases June 27- July 10 and July 11- July 24) national campaign on World Population Day per year, is done in all the states/ Districts. AYUSH Doctors are also trained in IUCD insertions. NSV Day (Non Scalpel Vasectomy Day) is conducted on the 21st of each month.
National family planning indemnity scheme (NFPIS) insures and indemnifies institutions against litigations in case of deaths, complications and sterilization failures.
Preventing Communicable and Non Communicable Diseases: National Disease
Control Programmes
A summary of the programmes are given below in the table.
| S. No. Programme Name | Key Functions |
| 1. National Program for Prevention and Control of Diabetes, CVD and Stroke (NPCDCS) | Specialized management of Diabetes, CVD, Stroke and Cancer. |
| 2. National program for Prevention and Control of Blindness (NPCB) | Providing screening for detection and management of diabetic retinopathy, refractory defects and glaucoma. |
| 3. National Program for Prevention and Control of Deafness (NPPCD) | Prevention of avoidable hearing loss and early detection & treatment of ear problems. |
| 4. National Mental Health Program (NMHP) | Providing services for early detection & treatment of mental illness in the community |
| 5. National Oral Health Program (NOHP) | Promotive and preventive oral health care at Primary and secondary level. |
| 6. National Program for Health Care of the Elderly (NPHCE) | Specialized accessible healthcare for elderly. |
| 7. National Iodine Deficiency Disease Control Program (NIDDCP) | To check iodine deficiency related health Problems. |
| 8. National Tobacco Control Program (NTCP) | To spread awareness and better implementation of tobacco control. |
| Communicable Disease Programmes | |
| 1. National Vector Borne Disease Control Programme (NVBDCP) | Prevention and control of vector borne diseases like malaria, Japanese encephalitis, dengue, chicken guinea, Kala-azar, Lymphatic filariasis. |
| 2. Revised National Tuberculosis Control Program (RNTCP) | Prevention, Control & Treatment of Tuberculosis. |
| 3. National Leprosy Eradication Program (NLEP) | Diagnosis and treatment (Multi-Drug Treatment- MDT) of leprosy patients. |
| 4. Integrated Disease Surveillance Program (IDSP) | Prevention and Control of outbreaks |
Community Processes : Institutionalizing Community- Led Action for Health
A summary of Community- Led Activities under NRHM is given below:
| S. Community Led No. Activities | Functions |
| 1. Village Health Sanitation & Nutrition Committee (VHSNC) | • Formed at each village level within the framework of Gram Sabha. • Subcommittee or a standing committee of the Gram Panchayat. • Representation of disadvantaged sections including women. • Acts as a platform for convergence of all departments at village level. It is also functions as a Planning and monitoring committee at the village level. |
| 2. ASHA | • Interface between the community and the public health system. • They are female health activists at household level. • Involved in educating and mobilizing communities particularly marginalized communities. • Functions include home visits, attending the Village Health and Nutrition Day (VHND), visits to the health facility, holding village level meetings and maintaining records. • In rural areas, one ASHA worker per village and in urban areas, one ASHA per 1000-2500 population. |
| 3. Anganwadi Workers | • Under the ICDS programme Involved with ASHAs and ANM( Triple A team) in convening the Village Health & Nutrition Days and VHSNCs. |
| 4. Jan Sunwai or Jan Samvad | • Public Dialogues/Public Hearings – taking direct feedback taken from the Community members • Grievance Redressal mechanism |
IEC Activities: Comprehensive communication strategy adopted with a strong behavior change communication (BCC) component in the IEC strategy; dissemination in villages and lowest levels. There is participation of non government agencies and professional and specialized agencies, visible mass media efforts in massive health communication efforts. There is a substantial portion of the interpersonal BCC effort is through local ground level workers including ASHA and ANMs, and community level structures equipped with communication kits, interacting on a one to one basis with families.
Convergence
- Convergence with Private Institutions and NGOs
A. PPP Mode: National Dialysis Programme33
This Programme enables for providing free dialysis services in District Hospitals on Public Private Partnership (PPP) Mode. The service provider provides medical and technical staff, dialysis machine and Reverse Osmosis (RO) Plant infrastructure while government provides Drugs, Water and Electricity and pays for the dialysis costs.
- Inter and intra sectoral Coordination: Convergence with Other Departments3536
A. Revitalization of local traditions: Mainstreaming of AYUSH
This includes co- location of AYUSH services at public health facilities including placing an AYUSH doctor at PHCs to strengthen Out- Patient (OP) services and setting up of separate AYUSH units/clinics at CHCs and District Hospitals. AYUSH doctors are trained and involved in Skilled Birth Attendant (SBA), IUCD insertion etc. and in preventive, screening and referral services under National Disease Control Programmes such as NPCDCS.
B. Integration with other programmes of Ministry of Health & Family Welfare [MoHFW]
MoHFW has large number of National Disease Control Programmes (Communicable and Non communicable) like RNTCP, IDSP, NVBDCP etc. All are brought under together in District/City/Village Plan so that preventive, promotive and curative aspects are well integrated at all levels and there is efficient and effective utilization of manpower and financial allocations under common District Health Society and availability of services at one point( UPHC).
C. With National Aids Control Organization (NACO):
NHM provides support to NACO programme implementation at district and sub- district levels. NACO provides counselors at CHCs and PHCs and testing kits as a part of NACP-III. Additional training is provided to existing medical officers and Para healthcare workers at lower levels on HIV/AIDS, condom promotion and Information Education and Communication (IEC) activities for better outreach.
D. Swachh Swasth Sarvtra:
Joint initiative with Ministry of Drinking water and Sanitation (MDWS), is to complement initiatives of Kayakalp and Swachh Bharat to make India free of Open Defecation and have safe drinking water.37 Convergence at the level of Panchayati Raj Institutions (PRIs), a common VHSNC, and common ASHA workers looks into the all these aspects.
E. Ministry Of Women And Child Development
Anganwadi Centre is a major activity centre for health services in addition to ICDS activities. AWW and MAS to work as a team for promoting health and nutrition related activities
F. Convergence with the Education department and programmes such as SABLA for preventing early age at marriage for girls.
At Ministry level, interdepartmental Committee with Mission Director as Chairman, reporting to Empowered Programme Committee (EPC), is developed. Convergence at the level of Mission Steering Group (MSG) with representation of all concerned Ministries is also done for Review and Monitoring.
Source: